EDIPPP Intervention Reduces Conversion to Full-Blown Psychosis Among At-Risk Young People, Says RWJF-Funded Study
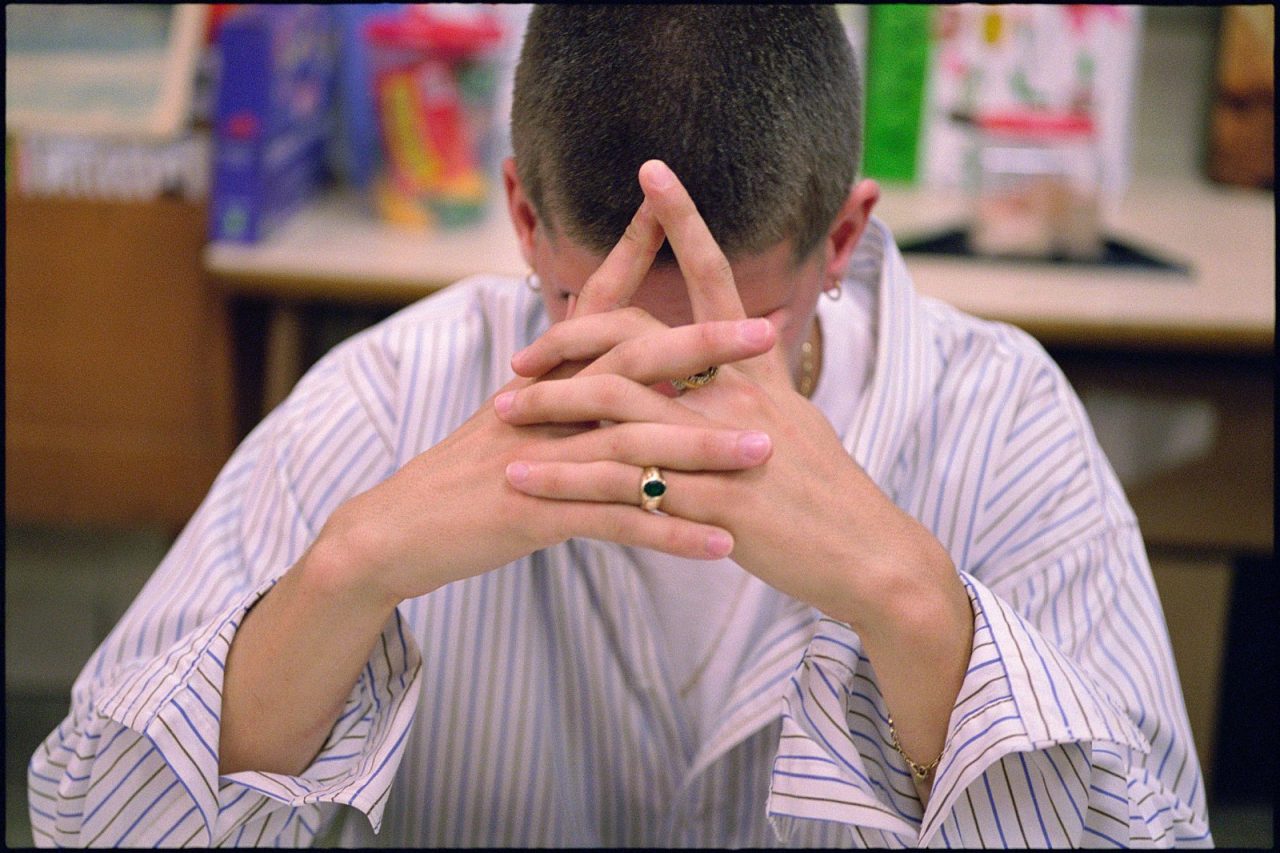
Princeton N.J.—Directly educating community members and actively involving families in treatment can avoid the onset of full psychosis among at-risk young people and keep them in school and working, according to a new Robert Wood Johnson Foundation-funded study. The national Early Detection and Intervention for the Prevention of Psychosis Program (EDIPPP) demonstration shows how a package of pre-emptive services can prevent young people exhibiting the earliest signs and symptoms of a psychotic disorder from converting to full-blown psychosis—enabling them to continue working and attending school.
“The results strengthen the evidence that early intervention to prevent onset or progression of psychosis in youth is effective, warrants expansion of practice, and constitutes an advance for public health,” said researchers writing in the current online edition of Schizophrenia Bulletin. Early intervention, particularly prior to the onset of psychosis “could lead to a reduction in total burden of disease,” they add.
From 2006-2013, six EDIPPP sites in Portland, Maine; Albuquerque, N.M.; Salem, Ore.; Ypsilanti, Mich.; Sacramento, Calif.; and Glen Oaks, N.Y., participated in the RWJF-funded study to look at the effects of proactively educating thousands of community members, health professionals, and educators about the early signs of severe mental illness so they can identify and prevent psychosis before it starts. EDIPPP helps identify at-risk teens and young adults early, and gets them into immediate treatment. The study looked at whether multi-pronged, evidence-based treatment interventions that include community outreach and education, family guidance and support, ongoing educational, occupational and social support, and medications if needed can improve outcomes and positively impact a young person’s life. Although this approach had actually reduced incidence of first-episode hospitalizations by one-third in Portland, where it started, the EDIPPP study was an attempt to see whether the same results could be replicated in different communities, with diverse populations and attitudes toward mental health.
Lead study author and EDIPPP Director William McFarlane, MD, says this provides evidence that the EDIPPP model can work across a broad spectrum of communities and have tremendous impact on lives and dollars. Psychosis ranks as one of the top most disabling conditions worldwide. Treatment, lost productivity and other costs of schizophrenia alone top $61 billion annually.
The study compared two treatment options for 337 young people between the ages of 12-25 who were at risk of psychosis. The conversion rate to psychosis among those who received the EDIPPP intervention with strong family involvement averaged 6.3 percent—well below the 29 percent conversion among at-risk individuals who get infrequent or no treatment in the community. EDIPPP not only helps families learn how to engage and support someone with severe mental illness, but it also helps patients succeed in school and at work. In fact, a significant greater number of people in the study who received the broad EDIPPP interventions were able to increase participation in work or school, increasing productivity.
“The burden of mental illness on the U.S. is enormous,” says McFarlane. “Through this kind of early intervention, these young people were able to continue to be productive citizens, and not disabled by a mental illness.” California and Oregon have taken steps to replicate the EDIPPP model or a version of it. McFarlane says he hopes that this national study provides the evidence for many more states and localities to develop and invest in a more preventive model for those who are in the very earliest stages of a severe mental illness.
“These results show that we should not have to wait until young people become psychotic or suicidal to intervene,” says Jane Lowe, PhD, a senior advisor at RWJF. “We hope this study not only changes the way we think about how we treat serious mental illness but also offers a new model for how we identify and treat at-risk young people to improve their life outcomes so they can lead healthy lives.”
About the Robert Wood Johnson Foundation
For more than 40 years the Robert Wood Johnson Foundation has worked to improve the health and health care of all Americans. We are striving to build a national Culture of Health that will enable all Americans to live longer, healthier lives now and for generations to come. For more information, visit www.rwjf.org. Follow the Foundation on Twitter at www.rwjf.org/twitter or on Facebook at www.rwjf.org/facebook.